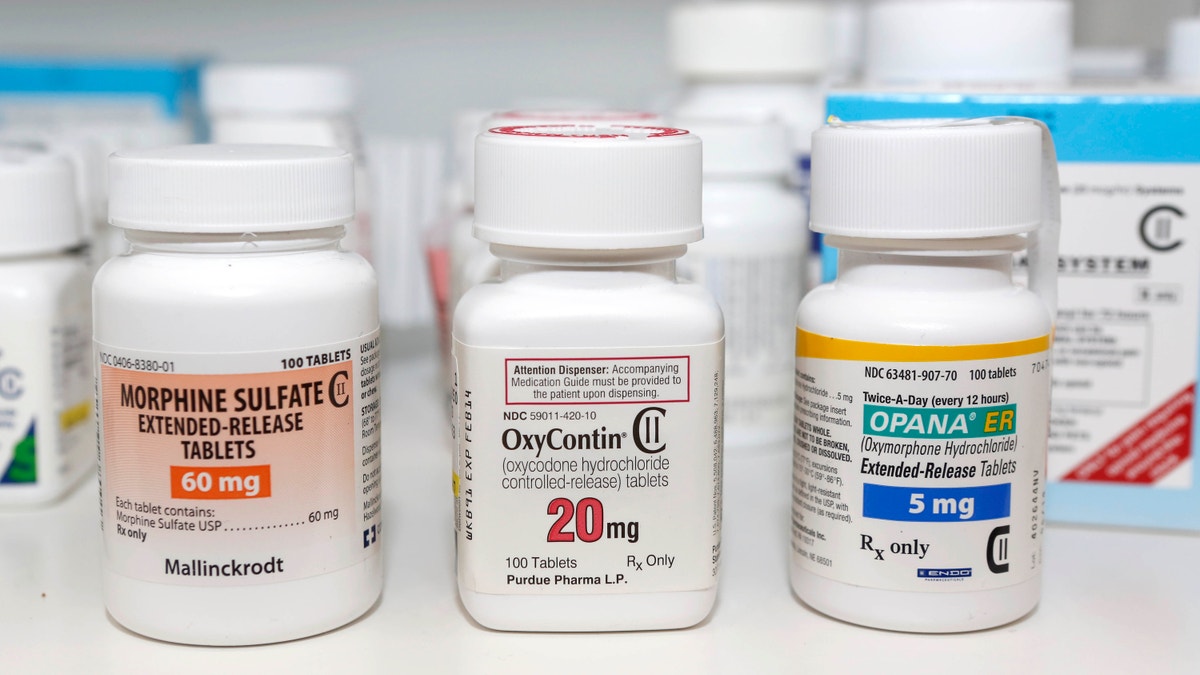
FILE - In this Jan. 18, 2013 file photo, Schedule 2 narcotics: Morphine Sulfate, OxyContin and Opana are displayed for a photograph in Carmichael, Calif. California doctors will be required to check a database of prescription narcotics before writing scripts for addictive drugs under legislation Gov. Jerry Brown signed Tuesday, Sept. 27, 2016, that aims to address the scourge of opioid abuse. (AP Photo/Rich Pedroncelli, File) (Copyright 2016 The Associated Press. All rights reserved.)
One of the most heartbreaking problems I’ve faced as CDC director is our nation’s opioid crisis. Lives, families, and communities continue to be devastated by this complex and evolving epidemic.
Year after year since I’ve been at CDC, the drug overdose death toll in our nation has been the highest on record. In 2015, more than 52,000 Americans lost their lives from an overdose. More than 33,000 of these deaths involved a prescription or illicit opioid.
This crisis was caused, in large part, by decades of prescribing too many opioids for too many conditions where they provide minimal benefit and is now made worse by wide availability of cheap, potent, and easily available illegal opioids: heroin, illicitly made fentanyl, and other, newer illicit synthetic opioids. These deadly drugs have found a ready market in people primed for addiction by misuse of prescription opioids.
Overdose deaths involving heroin have more than quadrupled since 2010. And what was a slow stream of illicit fentanyl, a synthetic opioid 50 to 100 times stronger than morphine, is now a flood, with the amount of the powerful drug seized by law enforcement increasing dramatically. America is awash in opioids; urgent action is critical.
This crisis was caused, in large part, by decades of prescribing too many opioids for too many conditions where they provide minimal benefit and is now made worse by wide availability of cheap, potent, and easily available illegal opioids: heroin, illicitly made fentanyl, and other, newer illicit synthetic opioids.
How to end the opioid overdose epidemic
Our nation’s current situation reminds me of a story often told to students of public health: A person on a riverbank saves one drowning person after another, before stopping, exhausted, to think: How can I stop people from falling into the river?
It is urgent and critical that we rescue people whose lives are at immediate risk. First responders and community members are increasingly administering naloxone, a drug that rapidly reverses an opioid overdose in progress. Increasing access among first responders and expanding programs that train community members on naloxone can save more lives.
Federal and state governments are also increasing access to opioid use disorder treatment, with medication-assisted treatment, an effective combination of behavioral therapy and medications.
More providers need to be trained and offer this evidence-based, life-saving treatment. We must also support our law enforcement partners in their efforts to make illicit opioids more expensive and harder to get.
While we implement these emergency response strategies, it is also important that we look upstream and prevent opioid use disorder in the first place —this starts with improving how providers prescribe opioids for pain treatment. CDC’s Guideline for Prescribing Opioids for Chronic Pain is an excellent starting point. There are safer drugs and treatment approaches that can control pain as well or better than opioids for the vast majority of patients. We must reduce the number of Americans exposed to opioids for the first time, especially for conditions where the risks of opioids outweigh the benefits. In addition, state policies should facilitate better use of prescription drug monitoring programs.
We must not forget what got us here in the first place. Doctors’ prudent use of the prescription pad and renewed commitment to treat pain more safely and effectively based on what we know now about opioids—as well as healthy awareness of the risks and benefits among patients prescribed these drugs—can change the path of the opioid epidemic.




















